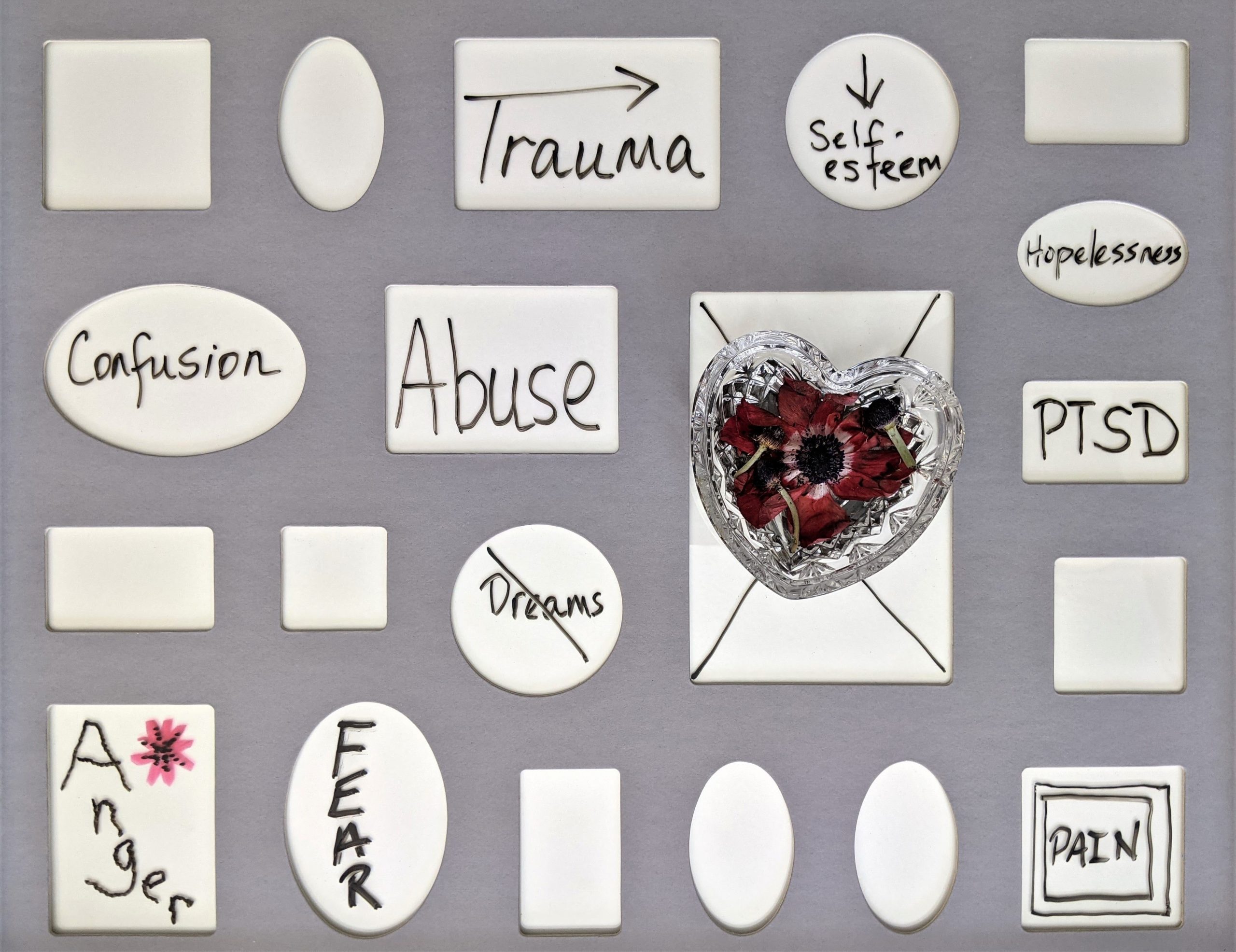
7 Signs You Are Suffering From PTSD

Disclaimer : Hey there, Psych2goers! Before we start, a friendly disclaimer, this article is not meant for a professional diagnosis or treatment. If you notice you or your loved ones experienced any signs stated below, please don’t hesitate to seek help from Psychiatrists or other mental health professionals.
Post-Traumatic Stress Disorder (PTSD) is a trauma and stress-related disorder that persisted for more than one month after exposure to an event or ordeal in which death or severe physical harm occurred or was threatened. Even the toughest and the most resilient among us is not immune to trauma. The traumatic events include motor-vehicle accidents, an active shooting in a public location, a narcissistic abuse in an intimate relationship, sexual assault, natural disasters, childhood abuse and neglect (Sweeton, 2013, Tanasugarn, 2020).
In the United States, approximately 8 million American adults developed PTSD and 3.5% of people including children were diagnosed with the disorder. The triggering event for this psychiatric condition may not be due to a single painful and troubling event but a series of incidents occurring over a period of time, for instance, the case with sexual or physical abuse during childhood. About 10 to 30 percent of war veterans develop the disorder. PTSD may often be accompanied by depression, substance use disorders and anxiety disorders.
Are you wondering what can be the signs indicating you are suffering from PTSD? Let’s delve into them below:
- You re-experience the intrusive upsetting memories of the traumatic event
You hear the blasting sound of the firecrackers, while driving in a neighbourhood, which suddenly triggers your memories of the wartime that you experienced in your home country. Your heart beats faster and you feel difficulty breathing. Suddenly, you slam on the brakes, pull your car to the side of the road, jump out and throw yourself into the ditch. The flashback is intense. Your experience is not of remembering an event, but of living the event.
Trauma survivors with PTSD often reported experiencing intrusive memories in the form of flashbacks, nightmares, and intrusive images. They describe experiencing posttraumatic flashback in the “here and now”, detached from the current reality and respond as if the trauma was happening at that moment (Ehlers, Hackmann, & Michael, 2004, Michael et., 2005). The intrusive memories are associated with “nowness” and they have been recognized by some as “warning signal intrusion” (Ehlers, Hackman, & Michael, 2004). These intrusive memories are neither random nor are they the most traumatic memories of the survivor. On the contrary, intrusive memories are memories that enable the trauma survivor to have a feeling that something unpleasant is brewing in the corner and is going to happen. Thus, there is functional significance in such memories, as they act as a way to warn for ensuing trauma events as well as serving as a signal when the situation or symptoms may exacerbate.
Intrusive memories are generally triggered by one of the five senses; vision, hearing, smell, taste and touch. When a person experiences such flashbacks, one’s autonomic nervous system is activated, causing faster respiration, increased heart rate, increased blood pressure, dilated pupils, pale skin color, and decreased digestion (for possible fight, flight or freeze response)(Ehlers et al, 2002).
2. You experience some type of dissociation

Fara (not a real name) grew up in a chaotic household. Her father was an alcoholic, violent man and would always beat Fara and her mother when he was drunk. One time, her father came home so drunk that he beat her mother to death. Since then, her father was arrested but Fara would always have daily flashbacks of the frightening incident. When she was asked about her trauma she would sometimes dissociate so strongly that she would seem to “forget” where she was.
Many people with PTSD may experience symptoms associated with reliving the traumatic event which include dissociative reactions or loss of awareness of present surroundings.
What does it feel like to dissociate?
Dissociation includes depersonalization and derealization.
Depersonalization is feeling detached or alienated from your body. A person might report the ultimate “out of body” experience such as not recognizing themselves in a mirror, feeling like their body is not their own, or even being temporarily unable to talk. For most people, they experience emotional numbing as well—feeling “meh” about things that should be emotionally intense.
Derealization refers to feeling isolated from your surroundings, such as being in the middle of a crowded party and feeling like you’re just invisibly watching it on TV. Apart from that, there is a sense that the world looks fake, or that they are observing it through a veil. Some say that the world loses color.
In children, however, dissociation can appear slightly different. They will be susceptible to trance states or blackouts, where they become unresponsive or have a lapse in attention. Apart from that, children may also stare at nothing, forget fragments of their life or what they were doing moments ago, or act as if they just woke up in response to being called to attention.
3. You avoid people, places, conversations, activities, objects, or situations that bring up memories of the event
You are a newly-recruited nurse in the Anaesthesia department. In the beginning of your career, you enjoy your job since you have a great team working alongside you. However, one day you are transferred to the emergency department, to help lessen the burden of handling the large number of patients admitted due to suspected COVID-19 infection. The stress level is building up, even some of the members of your team in the emergency department including the head doctor were infected. Left and right you saw patients were resuscitated and eventually passed away. Then you got to know the head doctor who was infected also passed away due to the infection. You grow tired, you feel a sense of avoidance, you want to avoid going to work altogether as whenever you stepped into the emergency department or whenever you saw the news about COVID-19 infection, you would feel your heart beat faster.
According to Jamie Marich, Ph.D., LPCC-S, LICDC-CS, trauma survivors with PTSD may experience avoidance symptoms, which represent an effort to withdraw from certain situations that bring about body-level distress or trauma-related symptoms. They may attempt to avoid external reminders such as people, places, conversations, activities, objects, situations) that arouse distressing memories, thoughts, or feelings about, or that are closely associated with, the traumatic event. These avoidance symptoms should be left open to individual meaning and interpretation as some reminders are very distinctive and unique. For example, a rape victim assaulted in a dry cleaning store at 10pm while walking home from work, may avoid the use of any cleaning products; may have panic attacks upon walking past facilities that smell like these dry cleaning chemicals; and may avoid a favourite restaurant because it happens to be situated along a dark alley, resembling the site of the assault.
4. You avoid thoughts, feelings, or conversations that bring up memories of the event

You are a survivor of a plane crash. Since then, you experience fear of flying and taking a flight is an emotional risk. You have concerns about the overwhelming, unbearable feelings on a flight and being unable to escape the plane.
People with PTSD may also avoid thoughts, conversations or feelings that can trigger memories of the event. It is common for the trauma survivors to report emotional avoidance as they view it as a form of escapism from painful or difficult emotions (Tull, 2020).
A research by Boden et al. (2013) reported that people with PTSD usually try to avoid or “push away” their emotions, both emotions about a traumatic experience and emotions in general. This avoidance behaviour may worsen PTSD symptoms or even contribute to the development of PTSD symptoms after experiencing a traumatic event.
5. You experience negative alterations in cognitions and mood
You have known a friend who has been sexually assaulted by her own boyfriend. Fortunately, she has removed herself from the abusive relationship, however, you notice she has persistent and elevated negative evaluations about herself, others, or the world. She will always say, “I am unlovable,”, “All men are evil,” and “The world is a scary place”.
Trauma survivors of PTSD may experience emotional numbing symptoms such as feeling detached from others, losing interest in activities they used to enjoy, or having trouble experiencing positive feelings such as happiness, joy or love. Apart from that, they might exhibit elevated self-blame or blame of others about the cause or consequence of the event. Patients may also experience a pervasive negative emotional state (ie shame, anger, or fear) (Tull, 2021).
6. You have trauma-related arousal and reactivity that began or worsened after the trauma

Fred (not a real name) was involved in a motor-vehicle accident half a year ago. He felt very sleepy as he was driving back home from a long shift at work. At some point of the journey, he experienced micro-sleep and during that moment he hit a man riding a motorcycle and caused his death. Since the tragedy, Fred is always “on edge” or “on guard”, finds it very difficult to relax or stay asleep and has trouble concentrating at work.
PTSD patients may experience arousal and reactive symptoms, such as being irritable and having angry outbursts; behaving carelessly or in a self-destructive way; being excessively vigilant of one’s surroundings; feeling easily startled; or having difficulty concentrating or sleeping (American Psychiatric Association, n.d.).
7. You experience distress or functional impairment
Can PTSD patients recover?
Yes they can.
A considerable number of people who develop posttraumatic stress disorder (PTSD) appear to experience spontaneous recovery or may recover with treatment (Bonanno et al., 2007).
How about their functional activity? Is it impaired?
PTSD sufferers may have difficulty functioning in their work or personal relationships. Traumatized children can experience trouble in school, become isolated from others and develop phobias (American Psychological Association, n.d.). However, trauma survivors of PTSD can also develop continual impairment in occupational and social functioning even after receiving specialized mental health treatment (Davidson et al., 2003). A research conducted by Westphal et al. (2011) reported that primary care patients with a history of past PTSD but without any other psychiatric comorbidity also develop significantly poorer mental health-related quality of life than their trauma-exposed counterparts without PTSD. Patients with past PTSD are inclined to fare better than those with current PTSD with regard to their ability to work, interact with their children, and mental health-related quality of life.
Final thoughts
You may have struggled with PTSD for many months or years, however this does not mean that you have to accept living with this condition forever. If for a physical disease, you keep finding a physician or treatments that are most suitable for you; a similar approach should also be applied when you are dealing with PTSD.
REFERENCES
American Psychiatric Association. (n.d.). What Is Posttraumatic Stress Disorder? What Is PTSD? https://www.psychiatry.org/patients-families/ptsd/what-is-ptsd
Boden, M.T., Westermann, S., McRae, K., et al. (2013). Emotion regulation and posttraumatic stress disorder: a prospective investigation. 32(3):296-314. doi:10.1521/jscp.2013.32.3.296
Bonanno, G.A., Galea, S., Bucciarelli, A., Vlahov, D. (2007). What predicts psychological resilience after disaster? The role of demographics, resources and life stress J Consult Clin Psychol. 75:671–682.
Davidson, J.R., Weisler, R.H., Butterfield, M.I., et al. (2003). Mirtazapine vs. placebo in posttraumatic stress disorder: a pilot trial. Biol Psychiatry. 53:188–191.
Ehlers, A., Hackmann, A., & Michael, T. (2004, July). Intrusive re-experiencing in post-traumatic stress disorder: phenomenology, theory, and therapy. Memory. 12(4),403-15.
Michael, T., Ehlers, A., Halligan, S.L., Clark, D.M. (2005, May). Unwanted memories of assault: what intrusion characteristics are associated with PTSD? Behav Res Ther. 43(5), 613-28.
Sussex Publishers. (n.d.). Dissociation. Psychology Today. https://www.psychologytoday.com/us/basics/dissociation.
Sweeton, J. (2013, July 4). Recognizing the Signs of Post-Traumatic Stress. Psychology Today. https://www.psychologytoday.com/us/blog/workings-well-being/201307/recognizing-the-signs-post-traumatic-stress.
Tanasugarn, A. (2020, June 3). How PTSD Affects the Quality of Your Life. Psychology Today. https://www.psychologytoday.com/us/blog/understanding-ptsd/202006/how-ptsd-affects-the-quality-your-life.
Tull, M. (2020, March 24). Why People With PTSD Use Emotional Avoidance to Cope. Verywell Mind. https://www.verywellmind.com/ptsd-and-emotional-avoidance-2797640.
Tull, M. (2021, June 3). Learn the Symptoms, Causes, and Treatment of PTSD. Verywell Mind. https://www.verywellmind.com/ptsd-in-the-dsm-5-2797324.
Westphal, M., Olfson, M., Gameroff, M. J., Wickramaratne, P., Pilowsky, D. J., Neugebauer, R., Lantigua, R., Shea, S., & Neria, Y. (2011, June 16). Functional impairment in adults with past posttraumatic stress disorder: findings from primary care. Depression and anxiety. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3647251/.






Responses